Colorectal Surgery
Anal Abscess
 An anal abscess is an extremely painful and potentially dangerous infection around the anus, typically of small anal glands. In addition to being extremely painful, these abscesses can spread infection to surrounding tissues and even in the bloodstream. Prompt treatment of anal abscesses is the best way to ensure you have a full recovery.
An anal abscess is an extremely painful and potentially dangerous infection around the anus, typically of small anal glands. In addition to being extremely painful, these abscesses can spread infection to surrounding tissues and even in the bloodstream. Prompt treatment of anal abscesses is the best way to ensure you have a full recovery.
Did you know?
It’s estimated that 50% of people with anal abscesses develop fistulas, which are small tunnels that make an abnormal and unhealthy connection between the skin and fistula.
Frequently Asked Questions
How do anal abscesses develop?
Anal abscesses can develop through a variety of methods. One of the most common is through the infection of an anal fissure – a small tear in the anal canal. Anal abscesses also develop through sexually transmitted diseases and through blocked anal glands.
Diseases like diabetes, colitis, and diverticulitis are also strongly linked to the development of anal abscesses.
The most common anal abscess is one that is located perianally. It’s most commonly seen as a boil near the anus that’s red, inflamed, and extremely painful.
What are the symptoms of anal abscesses?
Surface level or superficial abscesses are most commonly associated with throbbing pain that gets progressively worse, along with skin irritation around the anus and a discharge of pus. You may also experience constipation or a general aversion to having a bowel movement because of the pain.
If an abscess spreads you may experience a fever, chills, and an overall feeling of malaise. Oftentimes a fever is the sole symptom of a deeper infection.
What is the treatment for anal abscesses?
The most common treatment for anal abscesses is surgical cleaning and removal, along with antibiotics. This is not a condition you can treat yourself and must be addressed by a physician with experience treating anal abscesses.
Diverticular Disease
 Diverticular disease is an umbrella term used to refer to two separate colon disorders – diverticulosis and diverticulitis. In diverticulosis, pouches form and bulge within the colon, which usually does not cause symptoms. Diverticulitis occurs when these pouches become blocked with waste materials, causing them to inflame and become infected. Diverticulitis usually causes noticeable symptoms, such as abdominal discomfort and changes in bowel habits.
Diverticular disease is an umbrella term used to refer to two separate colon disorders – diverticulosis and diverticulitis. In diverticulosis, pouches form and bulge within the colon, which usually does not cause symptoms. Diverticulitis occurs when these pouches become blocked with waste materials, causing them to inflame and become infected. Diverticulitis usually causes noticeable symptoms, such as abdominal discomfort and changes in bowel habits.
Did you know…half of the people over age 60 and nearly everyone over age 80 has a diverticular disease? The condition is less common in young people, but the risk of developing it begins increasing at approximately age 40. At that time, chances of developing diverticular disease increase every decade. |
Frequently Asked Questions
What are the symptoms of diverticular disease?
People with diverticulosis are usually asymptomatic though diverticula pouches may bleed from time to time. The bleeding usually does not cause pain, though it can cause copious amounts of blood to appear in the stool. Diverticulitis, on the other hand, can cause acute attacks, resulting in pain, tenderness and cramps within the abdomen. Patients may also experience alternating bouts of constipation and diarrhea, and in some cases, chills or fever.
Why should I seek treatment for a diverticular disease?
Contact your doctor if you have any of the symptoms of diverticular disease. Always seek treatment for unexplained blood in your stool or for known diverticulitis-related bleeding that results in excessive blood loss or dizziness.
What are the treatments for diverticular disease?
Most people with a diverticular disease do not require any specific treatment. Dietary changes, such as eating plenty of fiber, are often enough to prevent complications. People with diverticulitis, however, may require greater interventions. This may include temporarily following an all liquid diet and taking antibiotics to prevent infection. In some cases, patients may need to undergo surgery to remove pouches from the colon that are bleeding or infected. Less often, a doctor may recommend removing the part of a patient’s colon that is subject to repeat diverticular infections.
Hemorrhoids
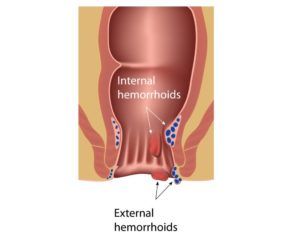 Hemorrhoids are incredibly common, with more than 3 million cases each year. They’re essentially swollen veins in the lowest part of your rectum and anus. Hemorrhoids are also known as piles.
Hemorrhoids are incredibly common, with more than 3 million cases each year. They’re essentially swollen veins in the lowest part of your rectum and anus. Hemorrhoids are also known as piles.
They become incredibly irritated when a person defecates. They’re one of the most common reasons for rectal bleeding and typically clear up within a few weeks.
Did you know?
Many people have hemorrhoids, but don’t know it. This is because oftentimes hemorrhoids don’t cause discomfort, particularly when they’re located internally.
Frequently Asked Questions
What’s the difference between internal and external Hemorrhoids?
Internal hemorrhoids are located so far inside the rectum that you can’t see them or feel them, due to the minimal amount of nerves in that region. They’re usually symptomless, with the only visible sign being slight bleeding.
External hemorrhoids are located around the anus and clearly visible. The opening of the anus has many nerve endings, which is why these hemorrhoids are often painful, particularly when you have a bowel movement. External hemorrhoids can prolapse, which means they get so big the bulge outside of the anal sphincter.
What causes Hemorrhoids?
Hemorrhoids are caused by pushing or straining during bowel movements. There is also a link between them and one’s genetics, meaning that if your parents or a close family member have had them you may be more prone.
Sitting or standing for long periods of time can also increase your risk of developing hemorrhoids.
How do I prevent them?
The best way to prevent hemorrhoids is by eating a diet rich in fruits and veggies. This increases your fiber intake and reduces the chance of constipation, one of the biggest reasons behind hemorrhoid development.
Treatment of hemorrhoids can be accomplished through a variety of over the counter options, including suppositories, witch hazel wipes, and creams that are applied to the opening of the anus.
Anorectal Fissure
 Anal fissures are tears in the lower portion of the rectum that cause pain and bleeding. Though irritating, anal fissures are common. They can last several weeks, however, if shorter than 12 weeks they’re known as acute anal fissures (short term). While these tiny tears can be frustrating, the good news is they are quite common and easy to treat.
Anal fissures are tears in the lower portion of the rectum that cause pain and bleeding. Though irritating, anal fissures are common. They can last several weeks, however, if shorter than 12 weeks they’re known as acute anal fissures (short term). While these tiny tears can be frustrating, the good news is they are quite common and easy to treat.
Did you know?
Anal fissures don’t discriminate based on age. They’re common to young and old, as well as healthy individuals.
Frequently Asked Questions
How do you diagnose an anal fissure?
Diagnosis is fairly easy but does require a physician. Typically a visual exam will suffice, however, a digital rectal exam or anoscopy. The anoscopy requires the use of a thin, lighted scope to look into the anal canal.
How do you treat anal fissures?
The key to treating anal fissures is prevention. By enjoying a diet high in fiber from veggies, fruits, and whole grains you can ensure your body is getting the fiber it needs. It’s also important to get plenty of fluids and at least 30 minutes of exercise a day.
If a lifestyle change doesn’t help, you may need to take a fiber supplement, which your doctor can recommend.
What are the causes of anal fissures?
These small tears are typically caused by passing a hard stool, repeated diarrhea, and childbirth. It’s suspected that extra tension in the anal sphincter can be to blame for fissures, however, anal intercourse and rectal exams can also cause them.
What are the symptoms of anal fissures?
The most common symptom of anal fissures is rectal bleeding. Typically patients will see a small bright bit of blood on the toilet tissue. If the stool is black or tarry that is a sign that there is upper gastrointestinal bleeding that should be immediately addressed by a physician.
Additional symptoms include a sharp stinging pain during bowel movements and excessive itching.